NUUMOON
Expertise & Treatments


Pediatric & Functional Orthodontics
It aims to consider the body as a whole and not to separate the functioning of the mouth from other parts of the body. Optimal jaw growth requires harmonious chewing, good swallowing, and optimal nasal breathing.
Thus, functional orthodontics takes an early interest in the body’s evolution for breathing and chewing. The orthodontist ensures the proper development of the dental arches.
For example, correcting an open bite solely with braces is highly likely to relapse! The cause of this open bite (tongue thrust, for example) must be addressed through functional re-education with the orthodontist or speech therapist.
Ventilation and Sleep
Orthodontics functional without braces all medical gentleness for a stability the long-term
The breathing pattern: often parents are not aware of their child’s nasal obstruction because this situation has been ongoing for a long time and everyone has become accustomed to it. And yet, this lack of nasal breathing, with its frequent rhinitis (more than three colds per winter), recurrent ear infections, restless sleep, and difficulties falling asleep lead to a significant deficiency in the development of the upper jaw.
This mouth breathing is aggravated by bad habits such as non-nutritive sucking (thumb or pacifier)! Indeed, the child keeps their mouth open, drools at night, has dry lips, their chin is often recessed, which leads to a growth disorder of the lower jaw; their tongue posture is altered, too high, too low, or too forward, resulting in a lack of contact between their teeth (open bite, for example).
And, of course, this breathing disorder is the origin of sometimes severe dysmorphoses such as major narrowness of the palate with significant dental crowding.
Anomalies functional
We like to see young children at the office, in order to be able to detect potential functional disorders. These disorders concern the child’s breathing, swallowing, chewing, and posture.
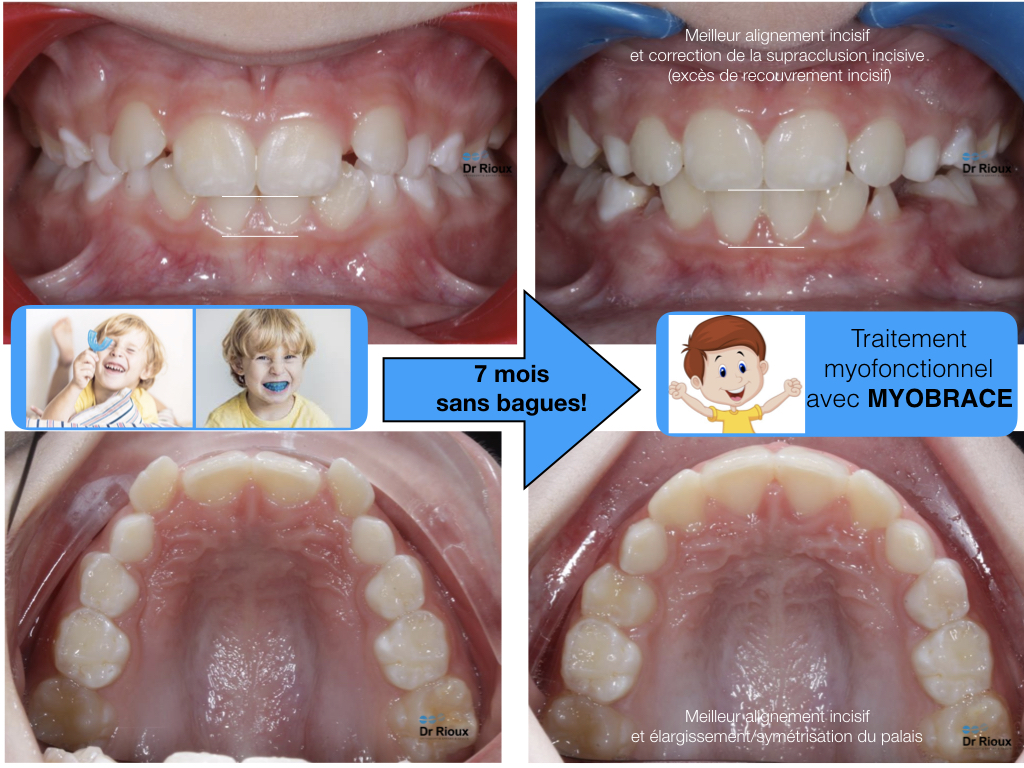
Very simple devices (small silicone trays) that are very fun allow our young children to:
- eliminate bad habits (thumb sucking, pacifier…),
- re-educate their functions and postures,
- restore a good jaw position
- and good dental alignment from the temporary dentition (baby teeth, 3-7 years).
More information on Myobrace
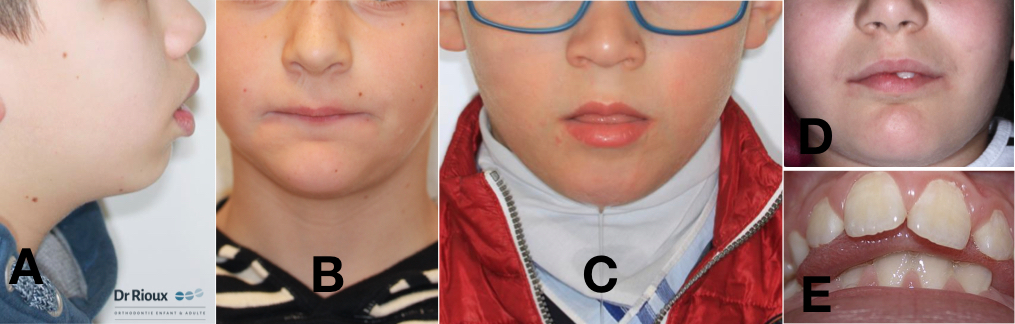
A. Labial hypotonia, oral breathing. B. Labial hypertonia. C. Labial hypotonia, salivary incontinence, low and forward tongue posture. D. Lower lip interposition under an incisor. E. Dysfunctional (infantile) swallowing.
The treatment is less painful
Myofunctional orthodontic treatments can be presented as follows: wearing a gentle and fun orthodontic appliance 2 hours a day (in front of the TV, during homework or car rides, etc.) and at night. Exercises are to be performed at home every evening. These are speech therapy exercises, and exercises aimed at improving the child’s general posture, their breathing (which should be nasal), and the quality of their sleep.
For better consideration of the natural evolution of teeth, functional orthodontics involves other professions. Thus the osteopath and the speech therapist help to naturally develop chewing, swallowing, and breathing functions.

Difference from conventional orthodontics
Here we are talking about interceptive orthodontic treatments : in other words, your child’s craniofacial growth is disrupted by functional disorders. This is highlighted during the orthodontic assessment. It may involve a low tongue posture, tongue thrust during swallowing (dysfunctional, infantile swallowing), lower lip interposition, digit sucking, mouth breathing…
Every 6-8 weeks approximately, your child will learn to re-educate the defects that hinder their proper growth. Their cooperation is therefore a key element of the treatment!
These treatments generally last from 6 to 12 months. Once the re-education is complete, the teeth naturally position themselves on the dental arch, which is no longer constrained in width.
ENT and allergology consultation
Alongside the treatment of teeth and occlusion (the fitting of teeth), the child should be directed to an ENT consultation for clearing of the nasal airway. This intervention can take place between 2 and 6 years of age to recover optimal nasal breathing. Beyond this, the consequences mentioned below will set in due to facial growth. In 75% of cases, the ENT consultation indicates that everything is in order (no anatomical defect, obstruction, allergies, infections, etc.). It is then simply a bad habit acquired by the child: breathing through the mouth, with a low tongue posture. Re-education is necessary. Often, results are obtained after just 3 months of myofunctional treatment.
Thumbs and Pacifiers
The sucking reflex
Sucking is a natural and soothing reflex that the child already has in the mother’s womb, from the 12th week of life. At birth, the infant is endowed with a strong sucking reflex, which is not just used for feeding. Sucking also causes the secretion of endorphins, which are hormones that provide a sense of well-being. Sucking therefore allows the infant to calm down, relax, fall asleep, and regulate their wake and sleep cycles.
Shortly after birth, the infant finds 1 or 2 fingers to comfort themselves and fall back asleep during the night. But it is also possible to offer them a pacifier, once breastfeeding is well established. Depending on their temperament, some babies will automatically calm down after feeds and will have little need to suck between them. Others will constantly need to suck to calm down. Children kept in daycare would develop more sucking habits than children kept at home.
According to a 2016 study: Alves FB, Wambier DS, Alvarez JH, da Rocha JC, Kummer TR, de Castro VC, Cabral H, Kozlowski VA Jr. Children using Day Nurseries’ Facilities can be Associated with more Risk to Nonnutritive SuckingHabits.J Contemp Dent Pract. 2016 Sep 1;17(9):721-727.
Pacifier
The pacifier is less harmful to the palate than the thumb during the first few months… Like the thumb, it soothes and calms the baby and helps them fall asleep. It promotes the pleasure of sucking and quickly becomes an object that reassures the baby.
The pacifier can be sterilized. The child can get rid of their pacifier more easily than their thumb, which would lead to fewer palate deformations. The child must feel ready to part with it…

Risks of the pacifier
The pacifier carries germs. It should not be systematically given to the child whenever they cry. Putting a pacifier too frequently in the baby’s mouth to prevent crying can become an overly systematic behavior that may have consequences on the child’s development.
The pacifier can prevent the baby from babbling if used too frequently. The child may become dependent on the pacifier. They may also lose it at night and start crying.
The risk of improper tooth positioning can be limited by choosing the right pacifier. For example, the MAM brand offers a Perfect MAM pacifier that we recommend. A long-term study confirms that this pacifier reduces the risk of improper tooth positioning compared to an ordinary pacifier, which is thicker at its base.
Wagner Y, Heinrich-Weltzien R. Effect of a thin-neck pacifier on primary dentition: a randomized controlled trial. Orthod Craniofac Res. 2016 Aug;19(3):127-36
Lower Jaw Growth
In our practice, we are advocates of undertaking early treatments, as soon as parents, the Dentist, the Pediatrician, or the Doctor detect a problem.
In all cases, a simple visit allows to clear up any doubt
In case of doubt, it’s better to consult the orthodontist too early rather than waiting and risking the problem worsening over time. The purpose of early orthodontic treatment is to:
- Quickly restore the child to an oro-facial environment favorable for harmonious facial growth with optimal musculoskeletal and dental function for their age,
- Simplify and shorten orthodontic treatment in permanent dentition (fixed appliances).
Early treatments are short-term treatments (about 6 to 12 months) and generally constitute the first phase of patient care. Indeed, more general dental disorders are corrected after all baby teeth have fallen out, in permanent dentition, using fixed multi-bracket appliances. This second phase lasts about 18 to 24 months and begins after a period of interruption or monitoring.
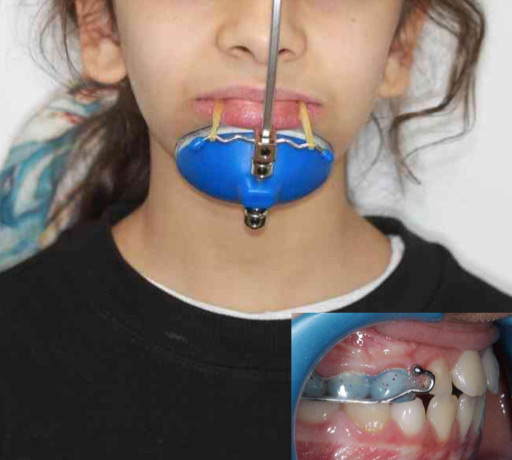
The appliances used during early treatment are generally removable appliances (expansion plates, functional appliances, nocturnal lingual envelope, bio-activators, etc.) and sometimes fixed (Expander, Quad-Helix, Bi-helix, etc.). Their action is often orthopedic, meaning they act on jaw growth.
Upper Jaw Growth
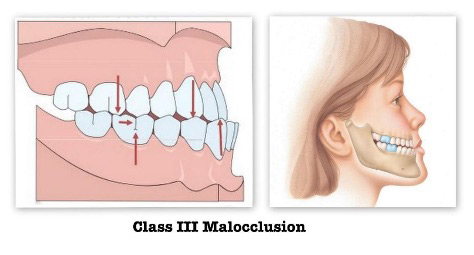
What is a Class III skeletal ?
Skeletal Class III is a syndrome, meaning that the misalignment of the jaws has multiple anatomical expressions. The most common anomaly is maxillary retrognathia, and not, as previously thought, mandibular prognathism.
The diagnosis of this anomaly is first clinical. It is made when we see the child in the waiting room: they have the typical face of retromaxillary with flattening of the nasolabial folds and upper lip, which is very characteristic. The diagnosis is then confirmed by X-ray. There is undoubtedly an often hereditary cause, but functions play a determining role.

Charles V (1500-1558) and his brother, as well as the Habsburgs, were known for their familial mandibular prognathism.
When should we treat a malocclusion “Class” III in a young child ?


We are often asked this question… Class III malocclusions and anterior crossbites are “spectacular” because they are very apparent and often constitute an aesthetic problem (in addition to being functional) from a very young age. Parents are more concerned about seeing such a malocclusion in their child than most other common occlusion problems (Class II, anterior open bite, crossbite, etc.).
The treatment is simple, and even more effective when undertaken early, in the primary dentition. The feasibility of“”intervening depends more on the ability to obtain cooperation from a very young patient than the indication to intervene. The nature of the treatment requires excellent cooperation from the patient for wearing appliances, maintaining them, etc., which is not easy at a very young age (3-6 years). This is why most clinicians prefer to wait at least until the eruption of the first permanent teeth (incisors, first molars) before intervening, which is around theage of 6-7 years.
However, if your child shows signs of a significant malocclusion at a young age (Class III or other problem), you can still consult an orthodontist to be reassured and obtain the necessary information on the subsequent steps that will ensure adequate follow-up and timely intervention.
It is not recommended to“wait until”adolescence to evaluate and begin treatment for Class III (especially severe cases) because they risk worsening over time and their treatment will be more complicated later (extractions, mini-screws, orthognathic surgery etc.).
If this malocclusion remains untreated it can lead to significant skeletal imbalances that can affect function, tooth wear, aesthetics and temporomandibular joints.
Functional “shift” of the mandible

- Class III cases are particular because they often have a functional component that makes them appear more severe than they actually are.
- There is often an interference between one (or more) upper and lower incisor that touch in an “edge-to-edge” relationship.
- The absence of contacts between the posterior teeth is unstable and uncomfortable for the child who cannot chew with their posterior teeth.
- This forces the child to advance the mandible to be able to chew properly using their posterior teeth which, in turn, creates an anterior crossbite (see photos). The term “functional” refers to the fact that it’s the function that “forces” the mandible forward.
- By moving the chin forward and sometimes to the side, the jaw deviation affects facial aesthetics much more than other types of problems.
- Note that we often blame the mandible as being responsible for the imbalance between the jaws when, frequently, this problem is actually caused by a deficiency of the upper maxilla. The maxilla being too far back creates the inadequate relationship between the incisors, which causes the mandible to advance as described above.
Eruption Problems
Panoramic X-ray and eruption prediction
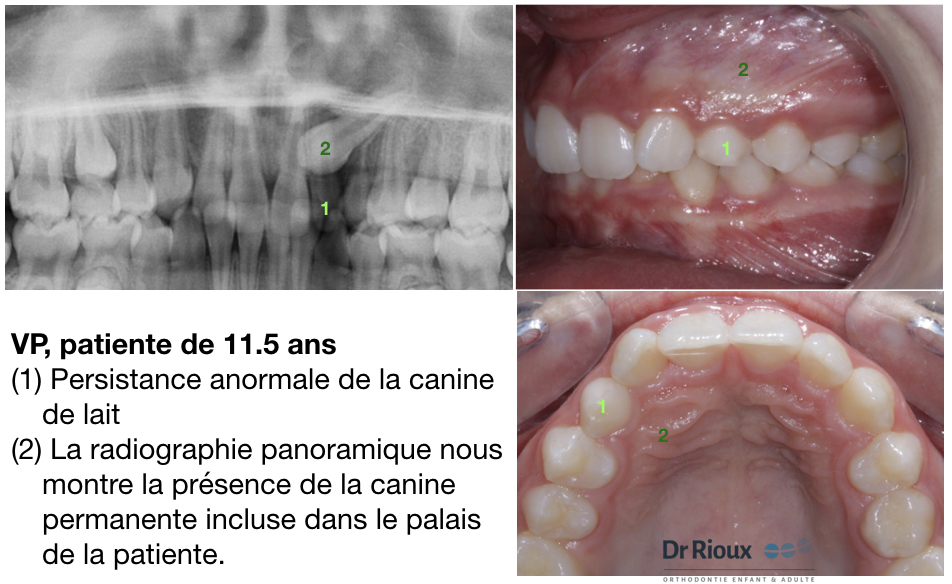
We too often see young adolescents arriving at the office with impacted canines. Their canine has not erupted and remained impacted, inside the palate bone or on the outer side of the alveolar bone. Most of the time, this is detected by their dentist during a routine check-up, with the persistence of the baby canine at an advanced age of the patient (A).
Is it possible to detect, predict and prevent the impaction of these canines? The answer is unfortunately YES. An abnormal direction of “canine eruption can be detected almost as soon as its crown and part of its root are formed, which can be from 7-8 years old for the earliest developing children. This does not mean that it is necessary to intervene immediately, but detecting this problem allows for appropriate monitoring and planning of intervention.
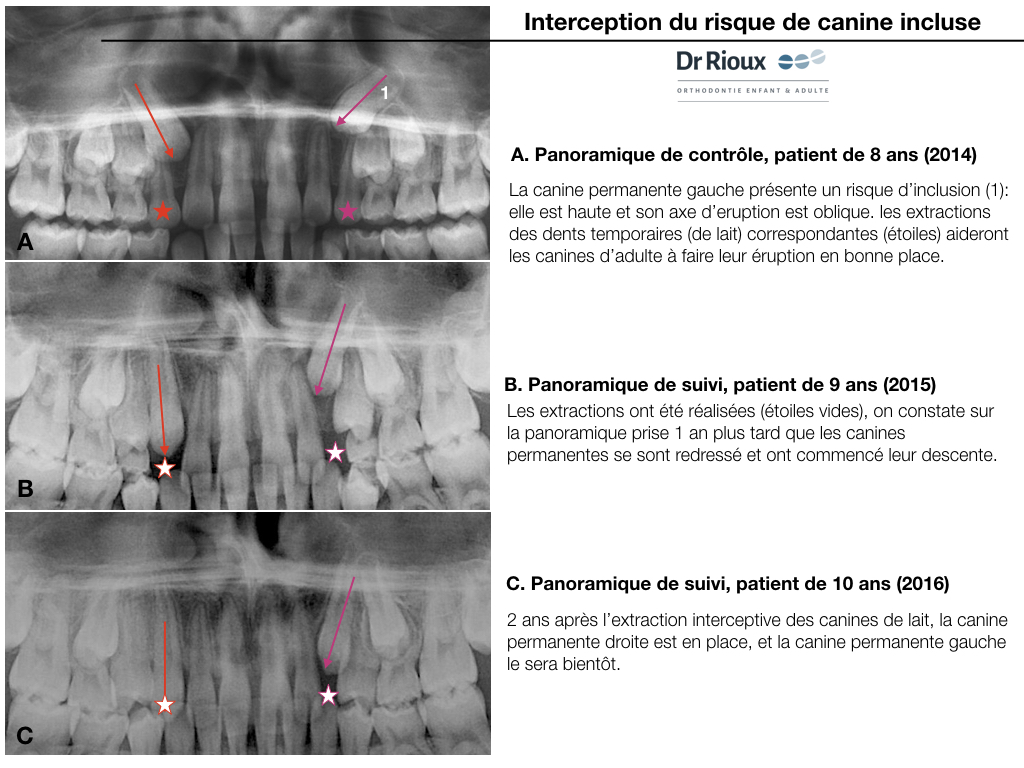
A panoramic X-ray allows us to” evaluate the position of the canines and predict their chances of “eruption. Extracting the temporary canines is the best way to influence the direction of” eruption of the permanent canines.
These situations could have been avoided
In the majority of cases, the presence of severely impacted canines in adolescents could have been avoided or at least minimized if adequate supervision and prevention had been done using panoramic X-rays and selective extractions.
To avoid such problems or minimize them, they must be detected early and the best way to do this is by taking a panoramic X-ray during the formation period of the canines but before they are too formed and too poorly positioned. Such an X-ray taken at the latest around 8-10 years old (depending on the characteristics of each case) constitutes a “crystal ball” allowing us to predict a good part of the dental and occlusion future of a young patient.
Interception terms the respect of impacted
Studies demonstrated, nearly 3 decades ago, the importance of taking panoramic X-rays to evaluate the direction of tooth eruption and the emergence of potential problems. Kurol is one of the pioneers in this field, but several similar studies have since confirmed his results. These works show the importance and reliability of using panoramic X-rays to evaluate the position of developing canines and their potential for impaction. A recent publication has confirmed these facts again.
The most effective interception measure to try to influence a canine that is developing ectopically is extracting the primary canine associated with the permanent canine. This requires an early diagnosis using X-ray(s) to evaluate the position of permanent canines and their relationship to adjacent teeth. When temporary teeth are extracted (canines and sometimes the first temporary molars), this eliminates a potential obstruction to the “eruption of the permanent canine, accelerates its eruption and usually improves its trajectory of” eruption, sometimes allowing the tooth to emerge normally. The success of the interception will depend on when this intervention is done and the position or malposition of the canine at the start.
References:
1- Ericson S, Kurol J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod 1988;10:283-295.
2- Sajnani et al. Early prediction of maxillary canine impaction from panoramic radiographs. AJODO Volume 142, Issue 1 , Pages 45-51 , July 2012
3- Lindauer SJ, Rubinstein LK, Hang WM, Andersen WC, Isaacson RJ. Canine impaction identified early with panoramic radiographs. J Am Dent Assoc. 1992;123:91–97
Palatal Expansion
The transverse deficiencies of the maxilla
Of high frequency (8 to 18% of patients in orthodontic consultation (Suri L, Taneja P. Surgically assisted rapid palatal expansion: a literature review. Am J Orthod Dentofacial Orthop. 2008 Feb; 133(2): 290-302. Review.)) and found in all dentitions, they are very often associated with functional disorders; these anomalies must be intercepted and corrected as early as possible due to the functional and aesthetic handicaps they cause and the absence of spontaneous correction.
These transverse problems are generally associated with vertical and anteroposterior problems, in syndromic or non-syndromic patients.

It concerns the “narrow” palate
Their etiology is complex and multifactorial. The causes can be congenital, genetic, environmental, growth-related, traumatic or iatrogenic. Contributing factors include a variety of craniofacial syndromes, thumb/finger sucking habits and mouth breathing during facial growth, as well as traumatic or surgical complications during cleft palate repair. The reported incidence of maxillary transverse deficiencies varies from 8.5 to 22% in children and adolescents.
Cross-bite or crossed bite
The most frequently reported clinical manifestations are unilateral or bilateral posterior cross-bites, palatal inclination of teeth, dental crowding, high palatal arches, narrow/tapered arch forms, and problems related to nasal breathing.
Expansion of the palate
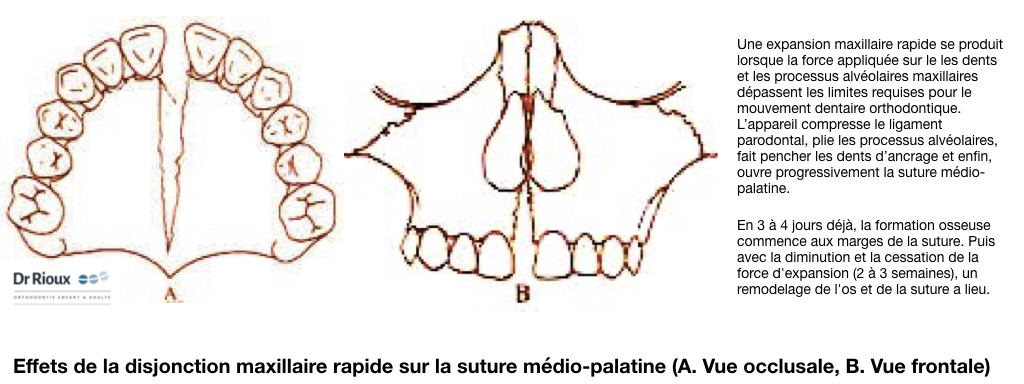
Correction of maxillary transverse deficiency usually requires palatal expansion through a combination of orthopedic (skeletal) and orthodontic movements. Three expansion modalities are used today. These are rapid maxillary expansion, slow maxillary expansion, and surgically assisted rapid palatal expansion.
Rapid maxillary expansion
Rapid maxillary expansion is probably the most popular modality among the three. Haas proposed in 1961 the use of fixed palatal expanders to quickly correct transverse disharmony in children and adolescents. According to the literature, non-surgical maxillary expansion improves ventilation, increases nasal cavity geometry, and decreases nasal airway resistance in children and adolescents (during growth).
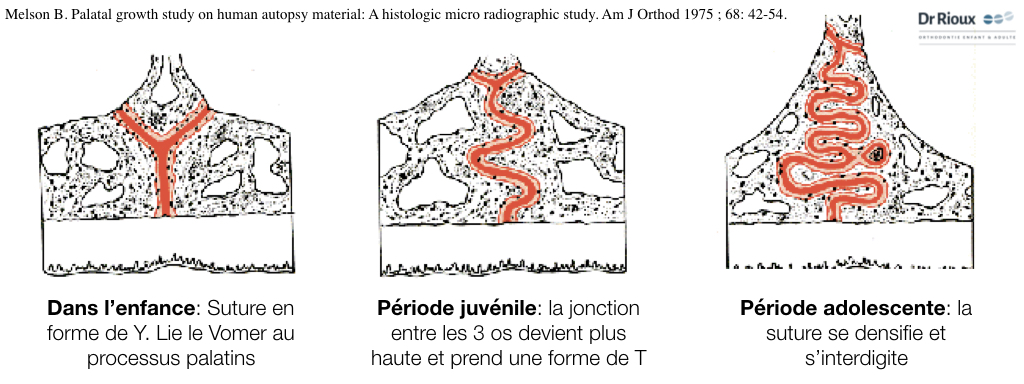
However, this does not work in adults. Their mid-palatal suture is already closed. Surgically assisted expansion is necessary. However, recent studies indicate that the maxillary suture is not fused enough to prevent the opening of the maxillary palatal suture in patients who are in their late teens or early twenties. Clinical, histological, and radiological evidence supports the use of non-surgical rapid maxillary expansion in young adults in their twenties. The pain experienced can be significant. Taking painkillers will decrease this discomfort. It is also possible to reduce the frequency of activations from 2 turns to 1 turn/day. Anterior ossification (at the level of the incisive foramen) is later. This must be taken into account during surgical release of the suture in cases of late management. Clinical, histological, and radiological evidence supports the use of non-surgical rapid maxillary expansion in young adults in their early twenties. The pain experienced can be significant. Taking painkillers will reduce this discomfort. It is also possible to reduce the frequency of activations from 2 turns to 1 turn per day. Anterior ossification (at the level of the incisive foramen) occurs later. This must be taken into account during surgical release of the suture in cases of late treatment.

Slow expansion or semi-rapid
The quad-helix, the loop arches and the Hawley or Schwartz plate allow for an increase in the transverse dimension of the maxilla as long as it is performed early. This mode of expansion is considered more stable because it allows for re-ossification and vascular development concurrent with the expansion. Slow expansion is indicated in cases where limited orthopedic effect is sought, without ENT objectives.
The earlier the transverse expansion, the less force is required to open the interpalatine suture. . The clinical studies of Wertz and Dreskin corroborate “Melsen’s histological study; expansion is easier and more stable in children under twelve years old. From” the age of twelve, there are more interdigitations or bone bridges between the two maxillae. Breaking these interdigitations to separate the maxillae requires significant force; this results in buccal tipping dental movements with a risk of bone fenestration and periodontal recessions, pain when activating the expansion device, and an increased risk of relapse despite overcorrection.
Surgically assisted rapid palatal expansion
Orthognathic surgery is indicated when a patient presents an orthodontic problem severe enough that compensation or camouflage treatments are no longer treatment solutions. The only possible treatment then becomes orthodontic-surgical. Surgery is not a substitute for orthodontic treatment. It is integrated into orthodontic treatment and must be coordinated with it and with other restorative treatments (implants, prosthetics, periodontology) if these are required. The surgery aims to reposition the bone bases face-to-face when there is too significant a discrepancy. In the case of transverse maxillary deficiencies, it involves surgically opening the palate to make it wider. This allows the lower jaw to fit correctly into the upper jaw when the patient closes their mouth. In addition to the aesthetic and masticatory impact, there is a significant positive ventilatory impact to consider.
There are two ways to widen the palate in adults:
- Widening the palate by segmenting the maxilla during a Le Fort I osteotomy
- Widening the palate using the principle of bone distraction (SARPE)

Orthodontics Smile Aesthetics
Conventional Braces
A discreet treatment
Adolescent orthodontic treatment with discreet external braces
Adolescent treatments no longer resemble what you knew in the 80s-90s!
Orthodontic treatments with digital assistance
Orthodontics in the 2020s is optimized by digital tools:
- during diagnosis,
- treatment planning,
- and then at the end of treatment for retention.
Do transparent braces turn yellow?
No! They are made of ceramic.
Will I have metal bits poking into my cheeks?
No! There’s no longer a need for metal or plastic “ligatures” to hold the wire in the braces.
Will I be in a lot of pain in the days following an appointment?
No! The wires used today (copper nickel-titanium alloys) deliver a slow and continuous force, close to physiological forces.
Invisalign®, Spark™ Aligners
A customized respect plan established for you
Before being able to establish a treatment plan, your orthodontist performs a clinical and radiological examination to verify if your teeth can be aligned with an Invisalign® or Spark™ orthodontic aligner system. After confirmation, a detailed treatment plan is then developed on a computer. This computerized process allows you to visualize the series of movements that your teeth will make during the treatment – so you can see the appearance of your teeth at the end of your orthodontic treatment even before you have started it.
How much will invisible orthodontic treatment cost?
Generally, the cost is comparable to that of traditional fixed appliances. The quote will be established after the diagnosis is made. Keep in mind that this is a MEDICAL treatment, so only an experienced and qualified practitioner is able to make a diagnosis and offer you an appropriate treatment.
Course of treatment sessions with aligners
The frequency of appointments is adapted to your treatment (usually every 6-8 weeks).
Designed to fit your lifestyle
The duration of treatment varies from person to person and depends on the complexity of each dental alignment problem. Easy to wear, cut along the gumline of the teeth, it doesn’t hurt and is completely invisible! Each aligner must be worn for 5 to 7 days, only removing it to eat and brush your teeth. Well-suited to your social life, this type of appliance can be removed from the mouth for a job interview, an exam, an appointment, etc.
Treatment time cut in half !
We can provide you with a treatment accelerator device, which is based on a safe technique that has been clinically approved for several years. This technology was initially, and for over 60 years, used in medicine for bone regeneration. It is documented in more than 3900 published articles. In addition to accelerating tooth movement, this device allows for a reduction in the discomfort caused by orthodontic movements. Its design makes it easy and comfortable to use, at home or while traveling, without changing your daily habits.
Lingual Braces
Doctors Rioux and Balland have a postgraduate degree in lingual technique.
For several years, they studied and treated numerous patients in Parisian hospitals, supervised by the pioneers and experts of this technique.
Advantages of lingual braces
- It is perfectly invisible: Bonded behind the teeth, it leaves the outer surface of your teeth perfectly bare and natural. You will see your smile align day by day.
- The appliance is made from digital impressions: They are taken at the office during a 30-minute appointment. Thanks to powerful software and a now-robotized manufacturing chain, the precision of this appliance is very good. This allows for considerable time savings in treatment. Here, the average treatment time is 18 months.
- There is a “light” version of the appliance, which is less expensive: If the treatment only concerns the front teeth, on either of your jaws, it is possible to partially brace your teeth. These “light” lingual technique alignment treatments last an average of 6 months.
- Cosmetic management of the treatment: When dental grinding is expected during treatment, or when there is an edentulous area to manage (for example, if the treatment requires the extraction of a tooth), a cover can be easily made. Only you and your orthodontist will know that a tooth is missing. This cover is removed once the edentulous space is closed orthodontically or prosthetically.
- Alignment from the first weeks of treatment: The first step of this type of treatment is to achieve initial tooth alignment. This occurs from the first weeks of treatment. Our patients thus quickly see the benefit of their treatment and regain their “self-esteem” more rapidly. You continue to live during your treatment, with teeth that are better and better positioned, without any visible appliance.
- Comfort of the appliance: At our office, we use the Incognito™ system, as the brackets are very round and comfortable for your tongue. External brackets can hurt your lips and cheeks. For internal brackets, the main discomfort is in the posterior area of the tongue. This discomfort disappears immediately thanks to orthodontic wax, which we will teach you how to use at the office. The majority of our patients are very surprised by the comfort of lingual braces. After a few days, it becomes part of your mouth, your daily life, as if it had always been there! Speech problems are not significant, or at least disappear relatively quickly. Oral hygiene problems are not greater than those encountered with vestibular technique.
Only a few orthodontists handle this type of appliance on a daily basis.
Indeed, mastering this technique requires additional training.
“We were fortunate to be able to practice lingual orthodontics in our hospital department during our studies, and we supplemented this training with a 2-year university diploma in Parisian hospitals. Very present at conferences, we love to re-learn, year after year, innovation after innovation, how to get the best out of this technique. As far as we are concerned, ‘lingual orthodontics is a true passion!’”
Dr. Rioux Dr. Balland

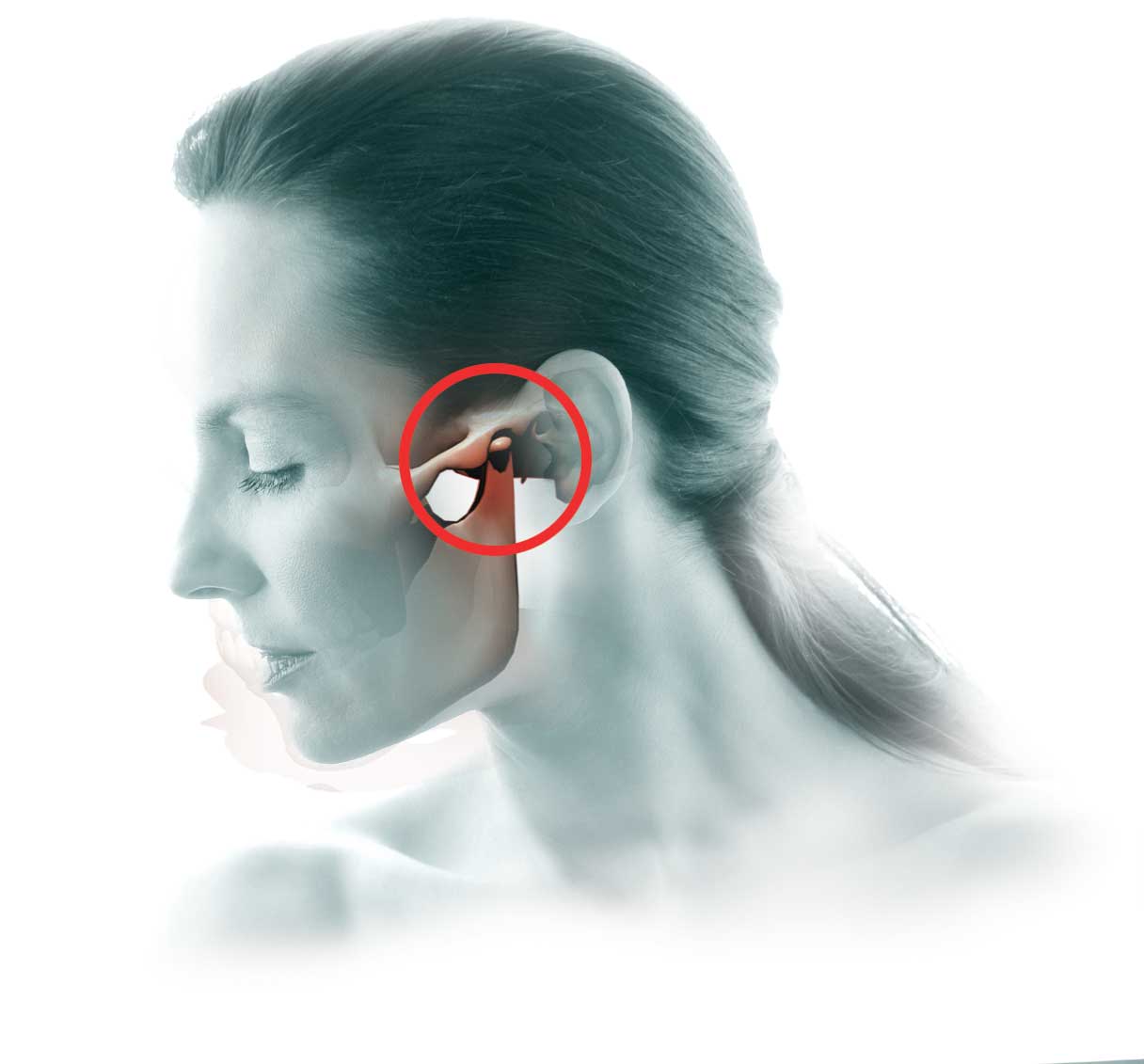
Temporomandibular Joint Disorders and Bruxism
The Symptoms
Do you suffer from unexplained headaches or jaw muscle pain?
Do you experience pain in the joint in front of your ear?
Do you suffer from discomfort and pain radiating into your neck and shoulders?
Do you hear “noises” or have sensations of cracking or popping in the joint when opening your mouth?
Perhaps you offer suffering from a temporomandibular joint disorder.
The temporomandibular joint (TMJ) is the joint that connects the lower jaw (mandible) to the skull bone. There are two of them, located on each side of the face, just in front of the ears.
These joints are among the most complex in the body. During their movements, they must open, close, slide forward, to one side and the other, in a synchronized manner. Many people have TMJ disorders, but only a minority will be affected by serious problems.
The TMJ disorders that may require treatment are those that:
- are accompanied by significant pain or discomfort,
- present reduced mobility (limited jaw opening).
The first step in the therapeutic approach is simply to allow the jaw to rest using easy-to-wear removable appliances.
Bruxism or Teeth Grinding/Clenching
Bruxism or teeth grinding/clenching
Bruxism (nocturnal or diurnal teeth grinding/clenching) is also a frequent reason for consultation and has multiple causes (stress, central nervous system dysfunction, muscle problems, dental occlusion issues…). An initial consultation with your orthodontist will help better identify the origin of your bruxism and evaluate the possibility of dental or joint action to relieve you.
Your case is unique, your orthodontist is here to inform you.

Dentofacial Orthopedics
To be Defined
A discreet treatment
Adolescent orthodontic treatment with discreet external braces
Adolescent treatments no longer resemble what you knew in the 80s-90s!
Orthodontic treatments with digital assistance
Orthodontics in the 2020s is optimized by digital tools:
- during diagnosis,
- treatment planning,
- and then at the end of treatment for retention.
Do transparent braces turn yellow?
No! They are made of ceramic.
Will I have metal bits poking into my cheeks?
No! There’s no longer a need for metal or plastic “ligatures” to hold the wire in the braces.
Will I be in a lot of pain in the days following an appointment?
No! The wires used today (copper nickel-titanium alloys) deliver a slow and continuous force, close to physiological forces.

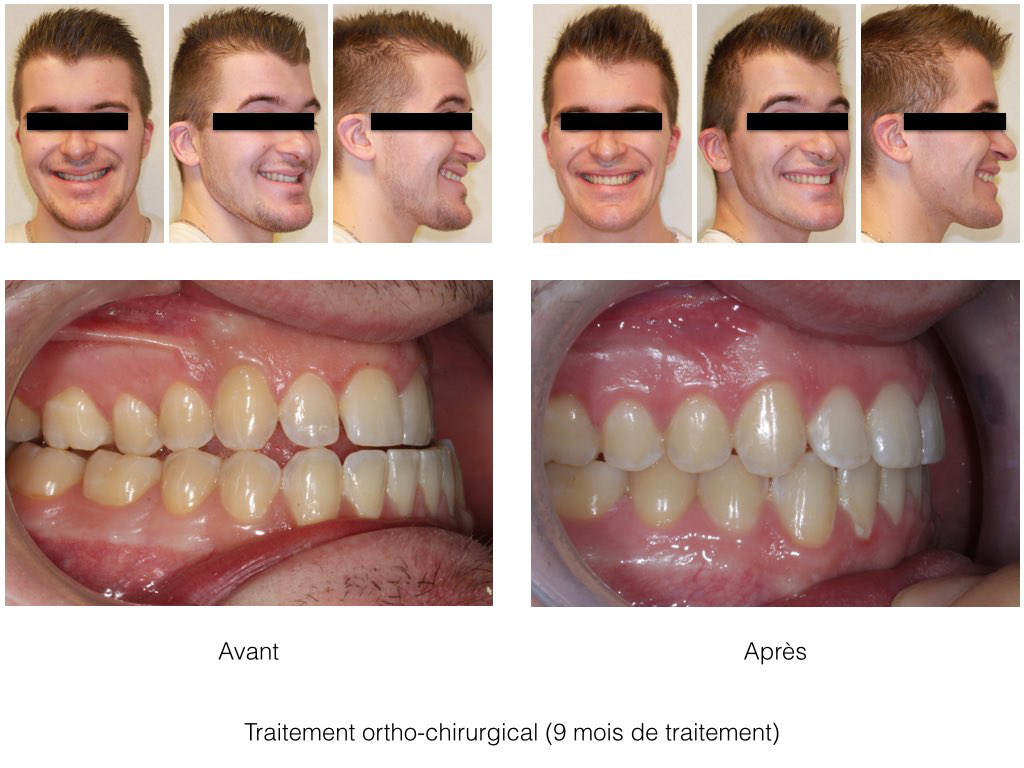
Orthognathic Surgery
For adolescents at the end of growth or for adults
A fundamental difference between adults and children or adolescents is the absence of growth.
In the presence of a significant skeletal imbalance between the jaws, it may be necessary to resort to jaw surgery to obtain an adequate balance between the upper and lower jaws.
Whereas in children, growth potential can be used to correct a skeletal imbalance, for example when one of the two jaws is too advanced or set back in relation to the other.
Close collaboration between orthodontist and maxillofacial surgeon
The necessity of combining orthodontics and maxillofacial surgery is now recognized by all. For about fifteen years, surgical-orthodontic protocols have evolved towards simplification, notably with the rise of digital planning and osteosynthesis materials.
The surgical indication is the result of a meticulous clinical and radiological study that combines knowledge from different specialties. The surgeon, general dentist, periodontist, orthodontist, as well as various other specialties (physiotherapy, osteopathy, speech therapy, ENT doctor, etc.) will decide on a therapeutic strategy at the beginning of the treatment.
The First Consultation
At the orthodontist’s
- Often, the first consultation takes place with the orthodontist. Either the patient is referred to us by their dentist or another doctor, or the patient comes on their own because they are aware of a dysmorphosis and wish to find a solution.
- It also often happens that the patient becomes aware of their skeletal discrepancy during this first consultation. The orthodontist will then inform them of the treatment possibilities, following their assessment.
- The assessment is necessary (photos, 3D dental impressions, X-rays, and analysis of these elements). Following a complete analysis, the orthodontist will be able to propose one or more treatment plans. When orthognathic surgery is indicated, the patient is invited to have a second consultation with the maxillofacial surgeon.
- If the patient refuses surgery, the orthodontist may choose therapeutic abstention if the cost/benefit/risk balance is not in the patient’s favor. A compromise treatment can also be proposed. Be aware that these treatments will never be as stable and lasting because the jaws will always be misaligned.
At the maxillofacial surgeon’s
Sometimes the patient first consults the maxillofacial surgeon. The latter will evaluate the malocclusion and explain to the patient the objectives of a possible surgery, the associated costs, steps, timelines, duration, risks, etc. so that the patient can make the most informed decision possible.
The vast majority of surgery cases require orthodontics to correct dental misalignments in order to prepare the case before surgery, so if the patient has not already consulted an orthodontist, the surgeon will direct them to an orthodontist for an initial orthodontic evaluation.

How Does the Procedure Take Place?
- The operation is performed under general anesthesia after a preoperative anesthetic consultation. In most cases, the maxilla is approached through incisions in the oral mucosa (no external scarring).
- The surgeon cuts the bone, which allows it to be moved in the direction planned during the intervention. The bone fragments are then fixed with titanium mini-plates (osteosynthesis) or sometimes steel or titanium wires.
- Sutures are placed in the mouth. They disappear in 2 to 4 weeks or are removed during a consultation.
- A blockage of the upper jaw with the lower jaw is often performed. The modalities and duration of the blockage will be specified by the surgeon.
- Bone consolidation is achieved after about a month and a half (6 weeks).
- Depending on the case, the osteosynthesis material can be removed a few months after the intervention (between 6 months and a year after the intervention).
Sagittal Anomalies
Skeletal Class II Malocclusions
Patient’s Request
Most often, the patient complains of having “upper teeth too far forward”, sometimes of having a “chin that is too small” or a “nose that is too big”. More rarely, the shape or interposition of their lips may bother them. If there is an overbite, it can damage the gums (palatal bite or gum recession in front of the lower incisors). In rare cases, snoring or even sleep apnea syndrome may motivate the consultation.
Skeletal Class II Malocclusion
This represents the majority of our patients. The lower jaw is set back relative to the upper jaw. There will be an associated dental discrepancy in the sagittal direction and sometimes also in the vertical direction (open bites, incisor overbite). Generally, this disorder is accompanied by a transverse insufficiency of the maxilla (maxillary endognathia) and a significant curve of the occlusal plane (called the curve of Spee).
How is the mandible advanced?
The mandibular osteotomy (Epker osteotomy, or Obwegeser or Dalpon) is performed from inside the mouth. The proximity of the inferior alveolar nerve explains the transient loss of sensation in the lower lip. The displacement of the mandible changes the position of the chin and lip.

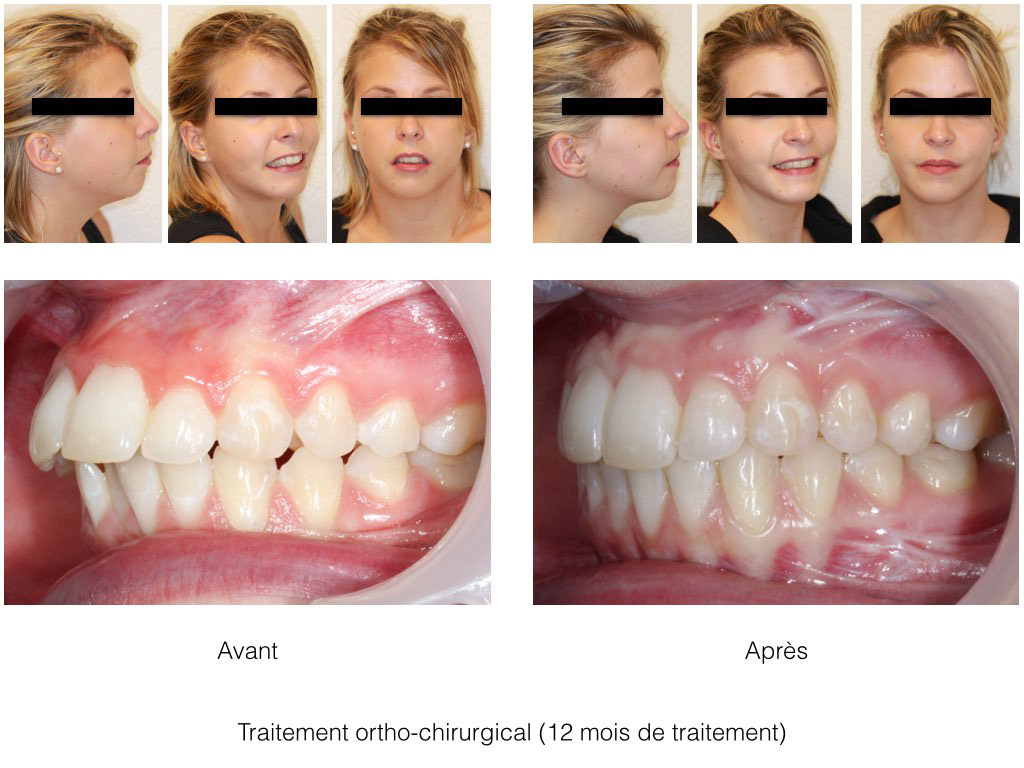
Skeletal Class III Malocclusions
Patient’s Request
In simplified terms, patients complain about their lower jaw being too “forward”. In some cases, it’s actually the upper jaw that is “set back”.
Skeletal Class III Malocclusion
By extension, skeletal class III malocclusions define trans-frontal profiles (“prognathic”), meaning the mandible is too far forward, or the maxilla is too far back. They are associated with a molar mesio-occlusion (Angle’s Class III), and often a reverse bite or an incisor “edge-to-edge” relationship. It is frequently associated with vertical excess of the face and transverse deficiency of the maxilla. The tongue volume and swallowing disorders should be considered before planning the procedure.
The surgical treatment consists, depending on the case, of advancing the maxilla or moving the mandible back, and often these two procedures are combined (bi-maxillary osteotomy). A genioplasty is often performed.
How is the maxilla advanced?
The maxillary osteotomy (Lefort I osteotomy) is performed from inside the mouth. The proximity to the nose allows for a modification of nasal breathing. The displacement of the maxilla changes the shape of the cheek grooves, the lip, and the position of the tip of the nose.
INSIGHTS
Content for children
